Abstract
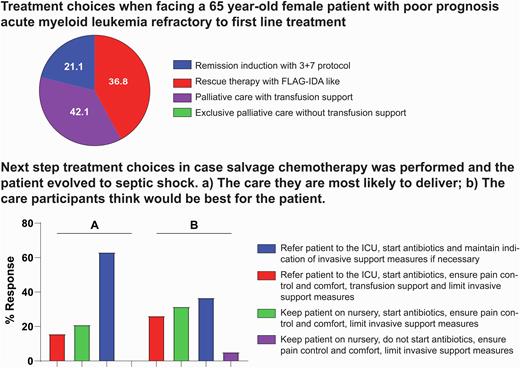
Introduction: Hematologic malignancies are a heterogeneous group of diseases with unique illness trajectories, treatment paradigms, and potential for curability, which affects patients' palliative care (PC) and end-of-life (EOL) care needs. EOL care is recognized as an under-researched area in the context of hematological malignancies. Several illness-specific, cultural and system-based barriers to palliative care integration and optimal end-of-life care exist in hematology patients. Adequate PC also requires appropriate knowledge from the healthcare staff, but frequently there are best-practice divergences within the same team, which may hinder integration and efficiency of patients' clinical courses. Objectives: We aimed to investigate characteristics of 19 hematologists and hematology residents from the hematology unit of the Federal University of Bahia's (UFBA) University Hospital and the variability in EOL care and opinions on PC. Methods: Descriptive cross-sectional study, conducted through the application of questionnaires. Variables were collected through a sociodemographic questionnaire and through the adaptation of clinical questionnaires used in previously published studies. Results: Preliminary data analysis was performed based on the application of questionnaires among 19 physicians working in a reference hematology unit of a university hospital in Salvador, Bahia, Brazil. Median age was 44 years old, 78.9% of participants were women, and 73.6% were graduated hematologists. When questioned about previous theoretical experiences on PC and/or EOL care during medical training, 57.8% reported experiences only during residency programs and 31.5% reported no previous training. Concerning a level of self-reported knowledge about PC, 57.8% defined as "regular" and 31.5% as "good." In the clinical questionnaire, participants were asked their hypothetical conduct when facing a 65-year-old female patient with poor prognosis acute myeloid leukemia refractory to first line treatment. Only 42.1% chose to establish PC with transfusion support, while 57.9% chose to follow other therapy regimens. Participants were also asked to consider a next step case salvage thought experiment for a patient experiencing septic shock following chemotherapy. Two options were prompted for selection: The care they are most likely to deliver or, the care they think is the best for the patient. There was a divergence between chosen strategies among 36.8% of participants. Reasons for this incongruence involved personal convictions (28.5%), legal aspects (28.5%) and other physicians' reactions (14.2%). Conclusion: Our study demonstrates the significant challenge of providing PC to patients with hematological malignancies, corroborating the international literature. Even within a team of specialists who have knowledge about PC, we observed divergences in their conduct in the face of a more complex clinical case. This demonstrates that PC, EOL and decision-making need to be further explored, requiring the urgent development of adequate education programs and best practices aimed at increasing and standardizing PC across institutions.
Disclosures
De Queiroz Crusoe:Janssen: Research Funding. Salvino:Libbs Farmacêutica: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal